Traumatic Acute Spinal Cord Injury Associated with Ossification of the Cervical Posterior Longitudinal Ligament without Tomographic Evidence of Bone Trauma. Case Series and Literature Review
Main Article Content
Abstract
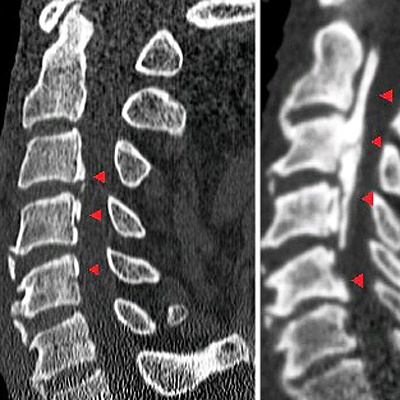
Materials and methods: We described a case series of patients with traumatic spinal cord injury and association of cervical OLLP, treated by our team during the period January 2012 - December 2019. We excluded patients with an association of vertebral fractures and/or dislocations, and those referred to another center before treatment and with incomplete records. Additionally, a narrative review of the literature on postoperative treatment and prognosis of this association was carried out. Ten articles were obtained with our search strategy for the narrative review.
Results: A sample of 5 cases was formed, all males, with an average age of 62.2 ( +/- 9.36), 4 cases were surgically treated by a posterior approach and 1 case was conservatively treated.
Conclusion: we presented a case series of a rare association in our region, preceded only by an isolated case report. The review of the current literature suggests timely surgical treatment over conservative treatment, but controversies persist in this regard.
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
Trauma 2017;31(Suppl 4):S7-S13. https://doi.org/10.1097/BOT.0000000000000943
2. Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can 2013;33(3):113-22. PMID: 23735450
3. Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, et al; American Association of Neurological
Surgeons; Congress of Neurological Surgeons. Guidelines for the management of acute cervical spine and spinal
cord injuries: 2013 update. Neurosurgery 2013;60(CN_suppl_1):82-91. https://doi.org/10.1227/01.neu.0000430319.32247.7f
4. Boese CK, Lechler P. Spinal cord injury without radiologic abnormalities in adults: a systematic review. J Trauma Acute Care Surg 2013;75(2):320-30. https://doi.org/10.1097/TA.0b013e31829243c9
5. Pang D, Wilberger JE Jr. Spinal cord injury without radiographic abnormalities in children. J Neurosurg
1982;57(1):114-29. https://doi.org/10.3171/jns.1982.57.1.0114
6. Gupta SK, Rajeev K, Khosla VK, Sharma BS, Paramjit, Mathuriya SN, et al. Spinal cord injury without
radiographic abnormality in adults. Spinal Cord 1999;37(10):726-9. https://doi.org/10.1038/sj.sc.3100900
7. Hendey GW, Wolfson AB, Mower WR, Hoffman JR; National Emergency X-Radiography Utilization Study Group.
Spinal cord injury without radiographic abnormality: results of the National Emergency X-Radiography Utilization
Study in blunt cervical trauma. J Trauma 2002;53(1):1-4. Disponible en: https://www.researchgate.net/profile/
Jerome_Hoffman2/publication/49600544_SCIWORA_is_Not_Just_Child’s_Play_Analysis_of_the_NEXUS_Data/
links/54171d200cf2218008bed0fd/SCIWORA-is-Not-Just-Childs-Play-Analysis-of-the-NEXUS-Data.pdf
8. Como JJ, Samia H, Nemunaitis GA, Jain V, Anderson JS, Malangoni MA, et al. The misapplication of the
term spinal cord injury without radiographic abnormality (SCIWORA) in adults. J Trauma Acute Care Surg
2012;73(5):1261-6. https://doi.org/10.1097/TA.0b013e318265cd8c
9. Yucesoy K, Yuksel KZ. SCIWORA in MRI era. Clin Neurol Neurosurg 2008;110(5):429-33. https://doi.org/10.1016/j.clineuro.2008.02.004
10. Boody BS, Lendner M, Vaccaro AR. Ossification of the posterior longitudinal ligament in the cervical spine: a
review. Int Orthop 2019;43(4):797-805. https://doi.org/10.1007/s00264-018-4106-5
11. Chikuda H, Seichi A, Takeshita K, Matsunaga S, Watanabe M, Nakagawa Y, et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine (Phila Pa 1976) 2011;36(18):1453-8. https://doi.org/10.1097/BRS.0b013e3181f49718
12. Endo S, Shimamura T, Nakae H, Takakuwa T, Yamada Y, Kasai T, et al. Cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Arch Orthop Trauma Surg 1994;113(4):218-21.
https://doi.org/10.1007/BF00441836
13. Fujimura Y, Nakamura M, Toyama Y. Influence of minor trauma on surgical results in patients with cervical OPLL. J Spinal Cord 1998;11(1):16-20. PMID: 9493765
14. Hayashi K, Yone K, Ito H, Yanase M, Sakou T. MRI findings in patients with a cervical spinal cord injury who
do not show radiographic evidence of a fracture or dislocation. Paraplegia 1995;33(4):212-5. https://doi:org/10.1038/sc.1995.47
15. Koyanagi I, Iwasaki Y, Hida K, Akino M, Imamura H, Abe H. Acute cervical cord injury without fracture or
dislocation of the spinal column. J Neurosurg 2000;93(1 Suppl):15-20. https://doi.org/10.3171/spi.2000.93.1.0015
16. Mizuno J, Nakagawa H, Hashizume Y. Pathology of the spinal cord damaged by ossification of the posterior
longitudinal ligament associated with spinal cord injury. Spinal Cord 1999;37(3):224-47. https://doi.org/10.1038/sj.sc.3100758
17. Koyanagi I, Iwasaki Y, Hida K, Imamura H, Fujimoto S, Akino M. Acute cervical cord injury associated with
ossification of the posterior longitudinal ligament. Neurosurgery 2003;53(4):887-92.
https://doi.org/10.1227/01.neu.0000083590.84053.cc
18. Gu Y, Chen L, Dong RB, Feng Y, Yang HL, Tang TS. Laminoplasty versus conservative treatment for acute
cervical spinal cord injury caused by ossification of the posterior longitudinal ligament after minor trauma. Spine J 2014;14(2):344-52. https://doi.org/10.1016/j.spinee.2013.06.083
19. Gu J, Guan F, Zhu L, Guan G, Chi Z, Li W, et al. Predictors of surgical outcome in acute spinal cord injury patients with cervical ossification of the posterior longitudinal ligament. World Neurosurg 2016;90:364-71.
https://doi.org/10.1016/j.wneu.2016.03.005
20. Onishi E, Sakamoto A, Murata S, Matsushita M. Risk factors for acute cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 2012;37(8):660-6.
https://doi.org/10.1097/BRS.0b013e31822da1d5
21. Okada S, Maeda T, Ohkawa Y, Harimaya K, Saiwai H, Kumamaru H, et al. Does ossification of the posterior
longitudinal ligament affect the neurological outcome after traumatic cervical cord injury? Spine (Phila Pa 1976)
2009;34(11):1148-52. https://doi.org/10.1097/BRS.0b013e31819e3215
22. Malpica RLM, Malpica RM, Fernández LCLG, Reyes LJ, Jiménez RHO. Osificación del ligamento longitudinal
posterior. Rev Esp Med Quir 2012;17(2):150-4. Disponible en: https://www.medigraphic.com/pdfs/quirurgicas/rmq-2012/rmq122p.pdf
23. Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for
neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med 2013;34(6):535-46.
https://doi.org/10.1179/204577211X13207446293695
24. Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res 1984;(184):71-84. PMID: 6423334
25. Yang D‐l, Zhang Y‐z, Shen Y, Cao J‐m. Surgical management of cervical cord injury with ossification of the cervical posterior longitudinal ligament. Orthop Surg 2011;3(2):95-101. https://doi.org/10.1111/j.1757-7861.2011.00131.x
26. Kwon SY, Shin JJ, Lee JH, Cho WH. Prognostic factors for surgical outcome in spinal cord injury associated with
ossification of the posterior longitudinal ligament (OPLL). J Orthop Surg Res 2015;10:94. https://doi.org/10.1186/s13018-015-0235-3
27. Hollenberg AM, Mesfin A. Ossification of the posterior longitudinal ligament in North American patients: Does presentation with spinal cord injury matter? World Neurosurg 2020;143:e581-e589.
https://doi.org/10.1016/j.wneu.2020.08.020
28. Choi JH, Shin JJ, Kim TH, Shin HS, Hwang YS, Park SK. Does intramedullary signal intensity on MRI affect
the surgical outcomes of patients with ossification of posterior longitudinal ligament? J Korean Neurosurg Soc
2014;56(2):121-9. https://doi.org/10.3340/jkns.2014.56.2.121
29. Wu JC, Chen YC, Liu L, Huang WC, Chen TJ, Lo SS, et al. Conservatively treated ossification of the posterior
longitudinal ligament increases the risk of spinal cord injury: a nationwide cohort study. J Neurotrauma
2012;29(3):462-8. https://doi.org/10.1089/neu.2011.2095
30. Li H, Jiang C. [Multivariate analysis of the operative effect on cervical spinal cord injury without fracture or
dislocation]. Zhongguo Gu Shang 2020;33(2):158-65. [En chino] https://doi.org/10.12200/j.issn.1003-0034.2020.02.014
31. Cabrera Rendón N, Fernández Albán M, Figueredo Méndez J, Salazar López A. Osificación del ligamento
longitudinal posterior cervical. Presentación de un caso y revisión de la literatura. CInvest Medicoquir 2020;12(2).
Disponible en: http://revcimeq.sld.cu/index.php/imq/article/view/612
32. Bazán PL, Borri AE, Medina M. Predictors in adult SCIWORA. Coluna/Columna 2013;12(4):326-9.
https://doi.org/10.1590/S1808-18512013000400014