Lumbar Decompression in Patients with Parkinson’s Disease: Series of Cases Treated with Minimally Invasive Surgery
Main Article Content
Abstract
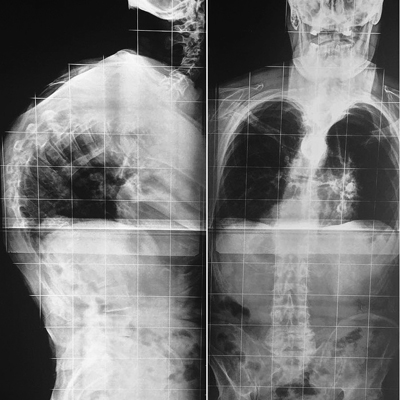
Materials and Methods: Surgically treated patients with a diagnosis of lumbar spinal stenosis and Parkinson’s disease were evaluated. The indication for the procedure was due to symptoms of the lumbar or foraminal stenosis of degenerative cause. All the patients were treated with decompressive surgery through a minimally invasive hemilaminectomy using tubular retraction and assistance with microscopy.
Results: From January 2015 to December 2017, 6 patients with Parkinson’s disease and lumbar spinal stenosis were treated. A total of 12 segments were decompressed, all patients were hospitalized for less than 24 hours. They did not require a transfusion nor suffered associated complications, with an average surgery time of 120 minutes. All with a minimum follow-up of 12 months and no relapse of the symptoms.
Conclusion: The high rate of surgical complications in patients with Parkinson’s disease, in contrast to the low rate of complications in the present study, suggests that minimally invasive surgery of the lumbar spine should be a surgical alternative in these patients.Level of Evidence: IV
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
dis- ease: construct failure and progressive deformity. Spine (Phila Pa 1976) 2004;29:2006-12.
https://doi.org/10.1097/01.brs.0000138306.02425.21
2. Boonstra TA, van der Kooij H, Munneke M, Bloem BR. Gait disorders and balance disturbances in Parkinson’s
disease: clinical update and pathophysiology. Curr Opin Neurol 2008;21:461-71. https://doi.org/10.1097/WCO.0b013e328305bdaf
3. Bourghli A, Guerin P, Vital JM, Aurouer N, Luc S, Gille O, et al. Posterior spinal fusion from T2 to the sacrum for
the management of major deformities in patients with Parkinson disease: a retrospective review with analysis of
complications. J Spinal Disord Tech 2012;25:E53-E60. https://doi.org/10.1097/BSD.0b013e3182496670
4. Melamed E, Djaldetti R. Camptocormia in Parkinson’s disease. J Neurol 2006;253(Suppl 7):VII14-VII16.
https://doi.org/10.1007/s00415-006-7004-5
5. Choi S, Kang K, Lee S, Lee S, Park M, Kim B, et al. The association of musculoskeletal pain with bone mineral
density in patients with Parkinson’s disease. J Neurol Sci 2015;357:e261-e262. https://doi.org/10.1159/000455009
6. Djaldetti R, Mosberg-Galili R, Sroka H, Merims D, Melamed E. Camptocormia (bent spine) in patients with
Parkinson’s disease—characterization and possible pathogenesis of an unusual phenomenon. Mov Disord
1999;14(3):443-7. https://doi.org/10.1002/1531-8257(199905)14:3<443::aid-mds1009>3.0.co;2-g
7. Mayer HM. Microsurgical decompression of acquired (degenerative) central and lateral spinal canal stenosis. En: Mayer HM (ed.). Minimally invasive spine surgery. Berlin, Germany: Springer; 2000:105-16.
8. Grimes JD, Hassan MN, Trent G, Halle D, Armstrong GW. Clinical and radiographic features of scoliosis in
Parkinson’s disease. Adv Neurol 1987;45:353-5. PMID: 3825710
9. Upadhyaya CD, Starr PA, Mummaneni PV. Spinal deformity and Parkinson disease: a treatment
algorithm. Neurosurg Focus 2010;28:E5. https://doi.org/10.3171/2010.1.FOCUS09288
10. Koller H, Acosta F, Zenner J, Ferraris L, Hitzl W, Meier O, et al. Spinal surgery in patients with Parkinson’s
disease: experiences with the challenges posed by sagittal imbalance and the Parkinson’s spine. Eur Spine J
2010;19(10):1785-94. https://doi.org/10.1007/s00586-010-1405-y
11. Moon SH, Lee HM, Chun HJ, Kang KT, Kim HS, Park JO, et al. Surgical outcome of lumbar fusion surgery in
patients with Parkinson disease. J Spinal Disord Tech 2012;25:351-5. https://doi.org/10.1097/BSD.0b013e318224a625
12. Oh JK, Smith JS, Sharey CI, Lafage V, Schwab F, Ames CP, et al. Sagittal spinopelvic malalignment in Parkinson
disease: prevalence and associations with disease severity. Spine (Phila Pa 1976) 2014;39:E833-E841. https://doi.
org/10.1097/BRS.0000000000000366
13. Galbusera F, Bassani T, Stucovitz E, Martini C, Maryem-Fama I, Berjano P, et al. Surgical treatment of spinal
disorders in Parkinson’s disease. Eur Spine J 2018 ;27(Suppl 1):101-8. https://doi.org/10.1007/s00586-018-5499-y
14. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation
and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine 2006;31:2329-36. https://doi.
org/10.1097/01.brs.0000238968.82799.d9
15. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using
sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 2006;31(3):303-8.
https://doi.org/10.1097/01.brs.0000197193.81296.f1
16. Watanabe K, Hirano T, Katsumi K, Ohashi M, Shoji H, Hasegawa K, et al. Characteristics of spinopelvic alignment in Parkinson’s disease: Comparison with adult spinal deformity. J Orthop Sci 2017;22(1):16-21.
https//doi.org/10.1016/j.jos.2016.09.013
17. Lamartina C, Berjano P.Classification of sagittal imbalance based on spinal alignment and compensatory
mechanisms. Eur Spine J 2014;23:1177-89. https://doi.org/10.1007/s00586-014-3227-9
18. Wunderlich S, Csoti I, Reiners K, Günthner-Lengsfeld T, Schneider C, Becker G, et al. Camptocormia in
Parkinson’s disease mimicked by focal myositis of the paraspinal muscles. Mov Disord 2002;17(3):598-600.
https://doi.org/10.1002/mds.10110